PROSTATE CANCER
- Home
- PROSTATE CANCER
PROSTATE CANCER TREATMENT & DIAGNOSIS
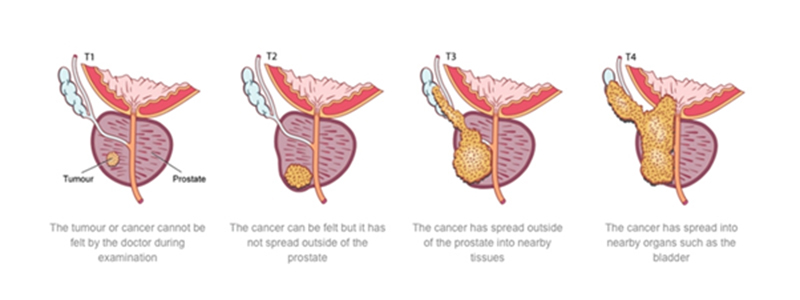
Adenocarcinoma of the prostate is the clinical term for a cancerous tumor on the prostate gland. As prostate cancer grows, it may spread to sac-like structures attached to the prostate (seminal vesicles), to tissues near the prostate, the interior of the gland, and to distant parts of the body (bones, liver, lungs, etc).
The prostate gland is located in the pelvis, below the bladder, above the urethral sphincter and penis, and in front of the rectum in men. It is made up of glandular tissue and muscle fibers that surround a portion of the urethra. The gland is covered by a membrane (called the prostate capsule) that produces prostate-specific antigen (PSA).
Early prostate cancer is usually discovered during a routine digital rectal xamination (DRE).
Symptoms are often similar to those of benign prostatic hyperplasia (BPH). Men observing the following signs and/or symptoms should see their physician for a thorough examination:
Preparing for Prostate Cancer Treatment
Radical prostatectomy is the surgical removal of the prostate gland and surrounding tissues including seminal vesicles and pelvic lymph nodes. Surgeons use one of two surgical techniques, retropubic prostatectomy or perineal prostatectomy.
General anesthesia is used in both procedures. In retropubic prostatectomy, an incision is made in the lower abdomen. This gives the surgeon access to prostate gland, seminal vesicles, and pelvic lymph nodes.
In perineal prostatectomy, the incision is made in the perineum (space between scrotum and rectum). With perineal prostatectomy, a second procedure is required to remove the pelvic lymph nodes, lymphadenectomy.